F105 The state of healthcare digitalization in Australia (Louise Schaper, AIDH)
Australia was in the global digital health-related news in 2018 of the national EHR project called My Health Record. The idea behind the project was to digitize the medical records of all the people from Australia. Today, 9 out of 10 Australians have My Health Record.
Australia has a national digital health strategy, which predicts that by 2022 the essential, foundational elements of health information that can be safely accessed, easily utilized, and shared will be in place. According to dr. Louise Schaper, CEO of Australasian Institute of Digital Health, there's been a lot of government commitment to invest in digital health. When the strategy was written, the government established an organization called the National Health Transitional Authority, now called the Australian Digital Health Agency. “This is a government-funded organization whose sole responsibility is to advance digital health,” explains dr. Louise Schaper.
Because the healthcare system in Australia relies heavily on community and health care consultation, the government put certain aspects of infrastructure in place. “We have a national identifier system in Australia. Every citizen that's getting health care has their own unique number just for that purpose. And then we also have another unique number for healthcare providers. Those unique numbers can be used in whatever health IT systems that are being built and designed and implemented in healthcare.”
My Health Record
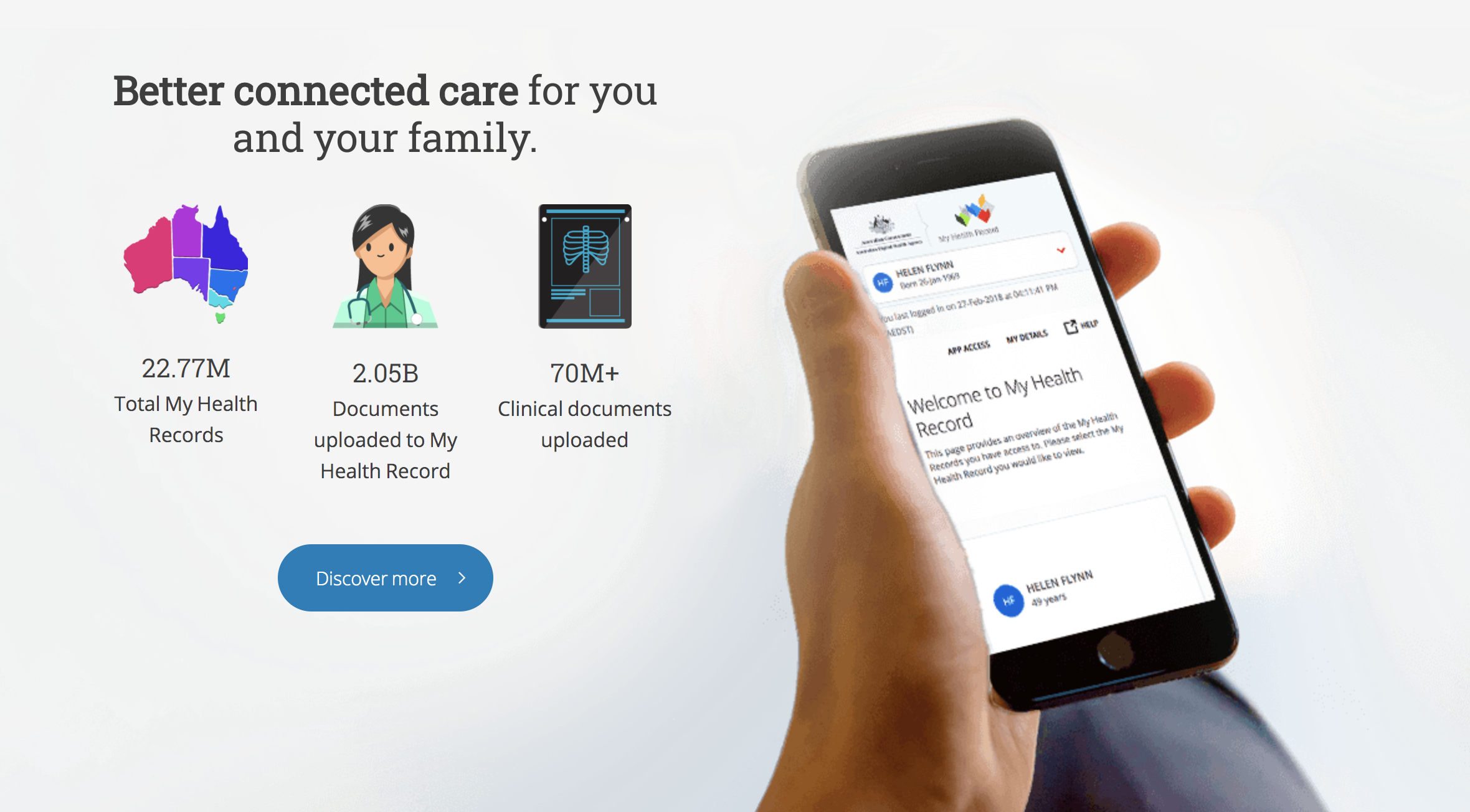
Australia was in the global digital health-related news in 2018 of the national EHR project called My Health Record. The idea behind the project was to digitize the medical records of all the people from Australia. Today, 9 out of 10 Australians have My Health Record. This means that all Australians have access to an electronic health record, which is a summary of their medical history.
“The idea is that when you go to see your general practitioner, or you have a stay in hospital, or you get blood tests, when you get a medication prescribed; all of those key activities are captured. The patient has full access and control over her record,“ says dr. Schaper.
Not everything is ideal though. While 98% of primary care practices are digitalized, that might not be the case with hospitals, mentions the CEO of AIDH: “The hospital sector is funded by state governments. Some states have embarked on significant programs of work to digitalize all of their hospitals. And they're in various stages of that. There are other states that haven't started yet. So obviously,if you want to connect to My Health Record as a health care organization, your information needs to be captured electronically. Since not everyone does that, the project is still very much a work in progress here.” An additional problem in incomplete My Health Records is that doctors that have access to the infrastructure, might not use it. “The only thing that guaranteed lands in the record is anything that the federal government has paid for. Because there is a financial aspect to it, that information which the government owns, that does get sucked in, and it's definitely in the My Health Record.”
Because of all this, the project is in a sort of Catch 22 situation - since records are incomplete clinicians can’t really rely on them and aren’t incentivized to send information in the system. At the same time, patients might not want to use the service, since the record is incomplete.
Dr. Louise Schaper.
The challenge in technology adoption
Dr. Louise Schafer did her Ph.D. in technology adoption among healthcare professionals. As she says, even though she finalized her thesis years ago, the findings are still applicable today. “Technology adoption boils down to one single thing - motivation. Even if a clinician is faced with a pretty poorly designed technology, which is painful to use, slows them down, or they have to use two different systems instead of one; none of that matters if the clinicians believes that capturing information electronically, and using that information in a digital form, will provide benefits for their patients. If that is the case, they're on board. If they believe that it will improve their practice as a clinician, and therefore enable them to provide better quality, higher quality patient care they will do things.”
She also warns that when hospitals do procure a digitalization system, the approach of introducing it to clinicians is often not well thought through: “The majority of clinicians are busy being fantastic clinicians. The first time they get introduced to an EHR is when their hospital buys an electronic medical record. Everyone gets told, ‘This is what's happening. Come to the training session on Friday, to get taught how to use the system, how the menus work, and where to put your information.’ So we approach it as training, exercise, and how to use a piece of software. Now, of course, training needs to happen. But the fact that we think that that is adequate, that it is all people need is wrong. One of the key focuses of the Institute of Digital Health is encouraging individuals as well as organizations to upskill people in digital health and health informatics beforehand. We can introduce these concepts first so that they understand the WHY. Things might be clunky, or they might take you longer to do what you used to do on paper faster. But by doing it this way, these are the benefits for the whole system and for your patients as well as for you. And if we start early and talk to people about that health informatics, that socio-technical lens behind why we should be doing things differently in health and bring it back to quality and safety for patients, then people go, ‘Oh, well, I get it. Now I get it.’”
Tune in for the full discussion.
Some questions addressed:
You have been the CEO of the Australasian Institute of Digital Health, for 11 years now. This means you were closely following the development of digital health from is very early stages to the full-blown development we see today.
Australia has a national digital health strategy, which predicts that by 2022 the essential, foundational elements of health information that can be safely accessed, easily utilized, and shared. How far is Australia from that goal? Did the COVID-19 pandemic accelerate achieving that goal?
We often treat Australia as one block, it is however divided into seven large regions. How much do they differ in terms of healthcare IT and digital health infrastructure? Is it possible to make a broad overview?
What is the state of the digitalization of healthcare institutions?
There are several entities in the space of healthcare digitalization - Medical Technology Association of Australia - the national association representing companies in the medical technology industry, ANDHealth - Australia's national digital health initiative, Australian eHealth Research Centre (AEHRC), Australian Institute of Digital Health which you are the CEO of. Can you describe a bit the relationships among these organizations, how do they differ, how much do you collaborate, does it make it easier to push progress because there are so many actors working in that direction, or is it more difficult because there are so many players?
A few years ago Australia introduced My Health Record - a key pillar in Australia’s National Digital Health Strategy. At first, it was a controversial project because of data-sharing related concerns. Now, 9 out of 10 people in Australia have My Health Record. More specifically, there are 22.8 million health records in My Health Record - Australia has 25 million people. What state is the project in today?
10% of people opted out. What does that mean? Are people on-board or just ignorant?
You have a Ph.D. in technology acceptance amongst healthcare professionals. I sense there’s a story there?
How would the PhD be different today? What changes are you noticing? Is the acceptance of technology event the right question? Sometimes healthcare professionals get a bad rep as being reluctant of technology, when in fact what they are reluctant to is technology not working well, computers freezing, software glitching, etc. …?
How can we increase the uptake of technologies, presuming the leadership is up for the change?